Dental implants are one of the best ways to replace missing teeth. However, many patients are concerned that having low bone density due to osteoporosis may prevent them from being suitable candidates for dental implant placements.
If you’re one of these patients, here are some answers to your concerns and questions about osteoporosis and dental implants.
What Is Osteoporosis?
Osteoporosis is a word that means “porous bones.” It’s a disease that decreases bone strength and mass, weakening bones and increasing your risk of suffering from sudden or unexpected fractures. Most patients don’t show any signs and symptoms or feel any pain until it causes painful fractures in the hips, wrists, or spine.
How Does Osteoporosis Occur?
Osteoporosis doesn’t have a known cause, but researchers understand its mechanisms. Bones are made of constantly-growing tissues. The inside of healthy bones is called trabecular bone, which looks like a sponge. An outer shell of dense bone called cortical bone wraps around the trabecular bone.
When osteoporosis occurs, the holes in the trabecular bone layer grow more frequently, thereby weakening the bone.
Bones are vital for our health and organ protection. They also store calcium and other minerals. They also become sources of these minerals that get broken down and rebuilt when the body needs them. This process is called bone remodeling, and it supplies calcium to the body while maintaining strong bones.
Normally, you build more bone than you lose before age 30. Bone loss occurs more than bone buildup once you reach 35. You also lose bone mass faster when you have osteoporosis. This occurs faster after menopause.
Osteoporosis and Oral Health
Osteoporosis affects your oral health in two ways:
Tooth Loss
Numerous studies have established the link between tooth loss and osteoporosis. While researchers are quite certain that osteoporosis is connected to tooth loss, they continue to investigate the nature of this connection.
One theory for this link is that your jawbone weakens and loses some of its density as osteoporosis progresses. Teeth lose some stability when the jawbone becomes weaker. These changes can affect teeth alignment, which could damage the roots of teeth and cause other oral health problems.
Osteoporosis Medications and Jaw Bone Health
Bisphosphonate therapy is the most common treatment for osteoporosis patients. They are usually given orally or through a vein to strengthen bones and prevent future fractures. According to the American College of Rheumatology, taking vitamin D or calcium with bisphosphonates is the best course to fight the adverse effects of osteoporosis.
Bisphosphonates and other antiresorptive medications like Prolia and dental implants don’t have a good relationship. They can damage your teeth and jaw and slow down bone healing. They are also linked with the development of a rare condition called osteonecrosis of the jaw (ONJ).
The likelihood of developing ONJ after dental surgery is high, especially in cancer patients who have received high-dose and long-term bisphosphonate therapy.
Anyone starting osteoporosis treatment using antiresorptive drugs like Reclast, Boniva IV, or Prolia should see their dentist before or shortly after. Together, you and your dentist can ensure the health of your teeth and gums before you start treatment and plan how to keep your mouth healthy during treatment.
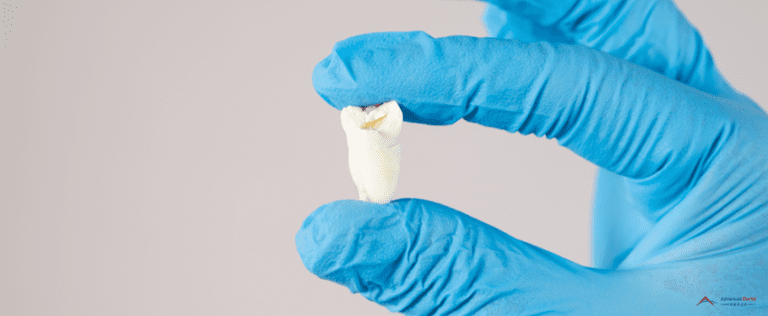
Osteoporosis and Dental Implants
How does osteoporosis affect dental treatments like dental implants? Osteoporosis can make your bones frail and can affect all the bones in your body. This also includes your jaw bones, which hold dental implants in place. Therefore, osteoporosis becomes a risk for dental implant treatments.
Can you have dental implants with osteoporosis? Yes, you can. Osteoporosis shouldn’t prevent you from getting implants. Research has shown that placing dental implants right after a tooth extraction is more successful.
Timing is essential when it comes to osteoporosis and dental implants. So don’t you fret as you can still have successful dental implants even if you have osteoporosis. Your dentist may recommend a bone transplant or mini-dental implants if you only have a small amount of bone loss in your jaw.
If you have osteoporosis, you should get dental implants as soon as possible or while still in its early stages; otherwise, you may reach a point where it’s too late to have them.
Also, keep in mind that dental implants and osteoporosis medications don’t go well together. Bisphosphonates may help slow down bone loss caused by osteoporosis, but they also slow down the jaw’s recovery after dental implant surgery. Some have also been linked to dental implant failure and removal. So make sure you disclose everything about your condition to your dentist before going through the implanting process.
How To Stay Healthy with Osteoporosis and Dental Implants
Keeping teeth and bones healthy is crucial when you have osteoporosis and dental implants. Here are some steps you can take to ensure your wellness:
Establish healthy habits.
Good habits that support your overall wellness keep your teeth and bones healthy. Some of these habits include:
- Consuming 600 to 800 IU of vitamin D every day
- Being physically active
- Eating a balanced diet
- Consuming at least 1000 to 1200 mg of calcium daily
- Limiting your alcohol consumption
- Quitting smoking
Talk to your doctor or nutritionist if you are experiencing any difficulty getting enough vitamin D or calcium from the foods you eat. Always follow directions when taking supplements.
Practice good oral hygiene.
Good oral hygiene is important for your teeth’ long-term health and well-being. Some recommendations from the American Dental Association (ADA) are:
- Cleaning between teeth with floss or interdental brushes
- Brushing teeth twice a day for two minutes
- Regular checkups with your dentist
- Brushing with fluoride toothpaste
- Reducing your consumption of sugary foods and drinks
Let your dentist know about your medications.
The ADA suggests that you don’t have to stop taking osteoporosis medication or skip the procedure. However, your dentist might need to make adjustments. Let your dentist know if you’re taking antiresorptive medications like bisphosphonates or other anti-inflammatory agents. This will allow them to adjust your treatment plan, which is especially important if you plan to have any dental procedures like tooth extraction.
Avoid damaging habits.
You can damage your natural teeth and dental implants by biting on hard candies, using your teeth to open bottles or food packets, and chewing on non-food items. Teeth grinding can damage your enamel and the crowns of your implants. Smoking also stains your teeth and increases your risk of developing gum disease. Avoiding these damaging habits as much as possible will keep your natural teeth and implants healthy.
Key Takeaway
Bone health is an essential aspect of osteoporosis and dental implants. Implants need strong bones to support them, which may get affected by osteoporosis since it’s a condition that weakens the bones. Some medications used to treat osteoporosis also put dental implants at risk of failure.
Osteoporosis shouldn’t keep you from having dental implants as long as your jaw is strong enough and you have them placed as soon as your teeth are extracted.
Stay strong and healthy with Advanced Dental Group.
Experience good oral care from our partner dentists in Dillon. They provide only the best treatments that suit your needs. Contact us today, and we’ll connect them to your right away.